Exercise and Insulin
Exercise and
Insulin
Our Top Tips
- Your starting blood sugar level matters as does regular checking during and after exercise.
- Carry identification.
- Use your diabetes team and dietitian – they can be great resources and have usually met lots of other people with diabetes who have successfully taken up exercise.
- A simple starting point is reducing your rapid-acting mealtime bolus insulin by 50% for the meal before you start exercise. If you did not adjust your insulin, then taking 30-60 grams of carb every hour during exercise helps to keep blood sugars in target and provides additional fuel for the working muscles.
- Check out our table (see Exercise and Insulin Adjustment).
- Remember, fluids are needed to prevent dehydration – water is best for low intensity exercise of short duration (less than 45 minutes) if your glucose levels are in your target.
- Sports drinks are helpful for more intensive training and for more prolonged endurance events (lasting more than an hour) – speak to your diabetes team beforehand!
- Things to keep in mind:
- Frequent monitoring of blood sugar levels.
- Adjusting both your basal (background) insulin and your mealtime rapid-acting insulin and carbs – insulin and carbs need changing during and AFTER exercise.
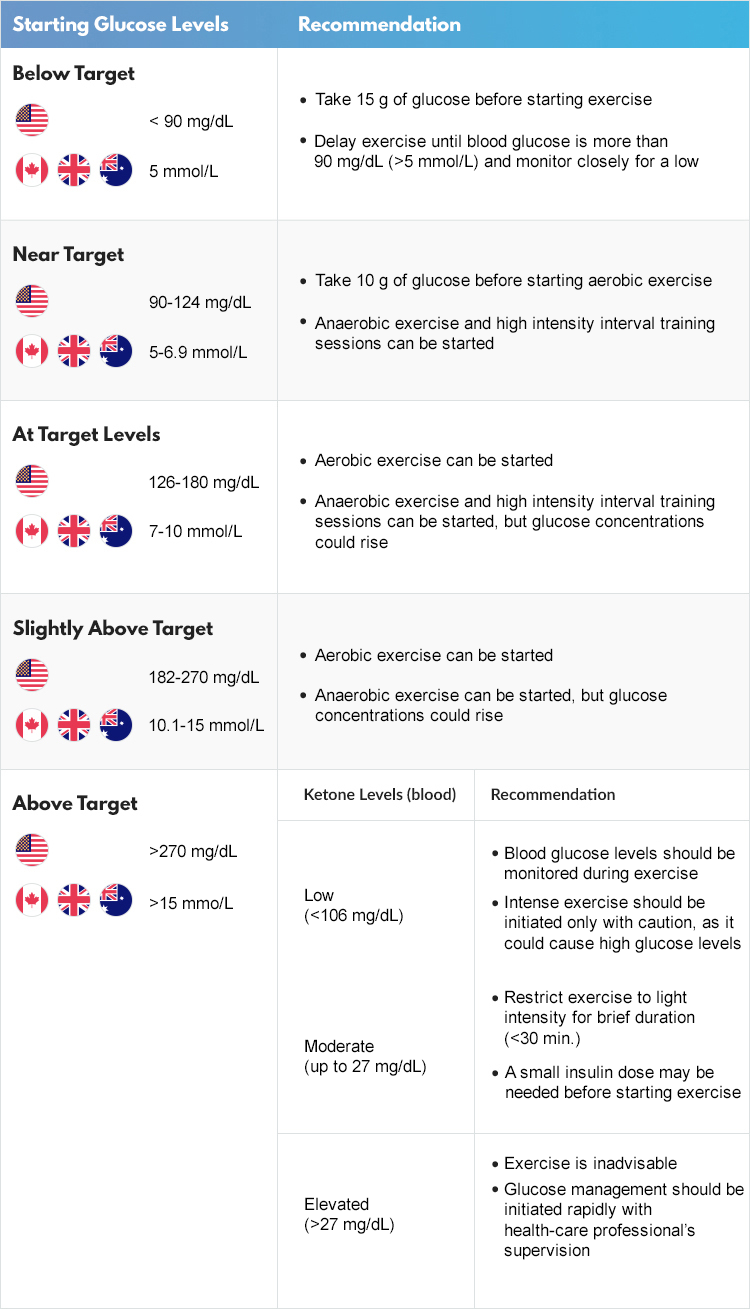
Blood glucose levels before you start
During most exercise (aerobic), muscles use glucose as a fuel. Under normal circumstances the liver releases glucose to help keep blood sugar levels elevated for the working muscles and brain. If insulin levels are not reduced (by lowering basal or bolus insulin) before the start of exercise, then the liver does not release enough glucose and blood sugar levels drop. This is when extra carbohydrates (ExCarbs) are needed – and you don’t take insulin for them!
Here are some recommendations: